Augmentative and Alternative Communication (AAC): Complete Guide for Families

Augmentative and alternative communication (AAC) includes tools, strategies, and devices that help children and adults communicate when speech alone is not enough. AAC may involve picture boards, sign language, speech-generating devices, or communication apps.
Used in early intervention, schools, rehabilitation, and medical settings, AAC supports individuals with autism, apraxia, cerebral palsy, stroke, traumatic brain injury, and other communication challenges.
This guide explains how AAC works, who benefits, device options, funding, and the role of speech therapy.ather than preventing it.
Table of Contents
Families often ask:
- Will AAC stop my child from talking?
- Is my child too young?
- What device is best?
- Will insurance cover it?
This guide answers those questions and provides a clear path forward.
What Is Augmentative Communication (AAC)?
Augmentative communication refers to methods used to support or replace spoken language.
AAC can be:
- No-tech – gestures, facial expressions, sign language
- Low-tech – picture boards, communication books, printed symbols
- High-tech – speech-generating devices and tablet-based apps
AAC supports both understanding and expression. Some individuals use AAC temporarily. Others use it long term.
The goal is always the same: meaningful communication.
Who Benefits From AAC?
AAC supports individuals of all ages.
Children who may benefit include:
- Children with autism
- Late talkers
- Children with childhood apraxia of speech (CAS)
- Children with cerebral palsy
- Children with Down syndrome
- Children with significant speech sound disorders
Adults may benefit after:
- Stroke
- Traumatic brain injury (TBI)
- ALS
- Parkinson’s disease
- Advanced neurological conditions
AAC is individualized. No two systems look exactly alike.
Why AAC Is Important in Speech Therapy
Communication is more than speech. It is connection.
When a child or adult cannot express needs, thoughts, or emotions clearly, frustration increases. Behavior may become challenging. Social withdrawal may occur.
AAC:
- Reduces communication breakdowns
- Builds vocabulary
- Supports sentence development
- Encourages social interaction
- Increases independence
Research consistently shows that AAC does not prevent speech development. In many cases, it supports spoken language growth.
Types of AAC: At a Glance
No-Tech AAC
- Gestures
- Facial expressions
- Sign language
- Body language
Low-Tech AAC
- Picture Exchange Communication System (PECS)
- Communication boards
- Choice boards
- Visual schedules
- Printed communication books
Low-tech systems are portable, affordable, and easy to customize.
High-Tech AAC
- Speech-generating devices
- Tablet-based communication apps
- Eye-gaze systems
- Touchscreen communication tools
High-tech systems provide voice output and often allow complex language building.
Low-Tech vs. High-Tech AAC: Quick Comparison
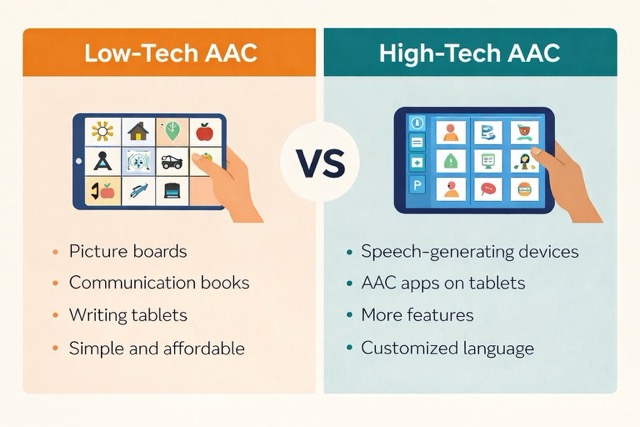
Low-Tech AAC
- No electronics required
- Affordable
- Easy to modify
- Durable
- No voice output
High-Tech AAC
- Electronic device required
- Voice output
- Greater vocabulary storage
- May require training and funding approval
A speech-language pathologist helps determine the most appropriate system.
Is AAC Appropriate for Young Children?
Yes. AAC can be introduced very early.
Children do not need to “prove” they cannot talk before receiving AAC support. Early communication access reduces frustration and supports overall language development.
Early AAC can:
- Encourage joint attention
- Build vocabulary
- Support early sentence use
- Improve social engagement
Early access leads to stronger outcomes.
When Should AAC Be Introduced?
AAC can be introduced when:
- Speech is limited or unclear
- Communication frustration is frequent
- A medical diagnosis affects speech development
- Progress in traditional speech therapy is slow
AAC does not replace therapy. It works alongside it.
The Role of Speech Therapy in AAC
A speech-language pathologist:
- Conducts an AAC evaluation
- Determines appropriate system type
- Trials devices when needed
- Trains families and caregivers
- Collaborates with schools
- Monitors progress
AAC success depends on consistent modeling and use across environments.
Speech therapy focuses on teaching how to use AAC meaningfully, not just how to press buttons.
What Happens During an AAC Evaluation?
An AAC evaluation may include:
- Review of medical and developmental history
- Assessment of speech and language skills
- Observation of communication attempts
- Trial of different AAC systems
- Collaboration with family and school
The goal is to match the individual with the most functional communication system.
Real-Life AAC Success
Many children begin with picture boards and later transition to high-tech systems. Some develop spoken language alongside AAC use. Others rely primarily on their device and communicate effectively in school, work, and social settings.
Communication growth often brings:
- Reduced frustration
- Increased participation
- Greater independence
- Stronger relationships
AAC gives individuals a voice — and sometimes changes the course of a life.
Real-Life AAC Success: Mary’s Story
In the early days of augmentative communication, access to devices was limited. One of the first individuals I supported was Mary, a pediatric nurse diagnosed with multiple sclerosis. As her speech declined, we developed a custom computer-based communication system — long before modern speech-generating devices existed.
Mary’s experience shows how augmentative and alternative communication (AAC) can restore independence, dignity, and meaningful connection.
👉 Read Mary’s Story: The Dawn of Augmentative Communication
Funding and Insurance for AAC
Funding options may include:
- Private insurance
- Medicaid
- State early intervention programs
- School-based services
- Nonprofit grants
High-tech devices typically require a formal evaluation and documentation of medical necessity.
Families should work closely with a speech-language pathologist experienced in AAC funding processes.
Frequently Asked Questions
Does AAC prevent speech?
No. Research shows AAC supports speech development. Many children increase verbal output once communication pressure is reduced.
Is AAC only for autism?
No. AAC supports many diagnoses and communication profiles.
Can AAC be temporary?
Yes. Some individuals use AAC short term while speech develops. Others use it long term.
What if my child resists the device?
Consistent modeling and guided use are essential. Resistance often decreases as communication becomes easier and more successful.
How to Choose the Right AAC System
Choosing the right system depends on:
- Cognitive skills
- Motor abilities
- Vision and hearing
- Communication needs
- Family involvement
- Environment (home, school, community)
No single system works for everyone. Individualization is key.
Related AAC Resources
You may also want to explore:
- AAC for toddlers
- AAC for autism
- High-tech AAC devices
- Low-tech AAC tools
- Speech-generating devices
- AAC funding and insurance guidance
Find a Speech Therapist Experienced in AAC
AAC implementation requires evaluation, device trials, training, and family coaching. Work with a licensed speech-language pathologist experienced in augmentative communication.
👉 Find a Speech Therapist Near You
Conclusion
Augmentative communication (AAC) provides access to language when speech alone is not enough. It supports connection, learning, and independence across the lifespan.
AAC is not about replacing speech. It is about opening communication.